Kaiser Permanente Washington Specialty Pharmacy: HIV & PrEP services. The objective of the Specialty Pharmacy’s HIV (human immunodeficiency virus) and PrEP (pre-exposure prophylaxis) services is to help you get maximum benefit from your medications and treatment plan. I wondering about that I got copies of my medicail from my cardiolist 5 years ago.recently I exprenced puting me off for an apointment 2 times and showed up then they said that could find me on the the appointment had to come back for 2 or 3 hours later.Then it was a bad stress test.The doctor wants to do a angiogram was told by the nurse that called.I not having any heart pains.I exercise.
Algorithm developed by Kaiser Permanente researchers could refer more at-risk patients for preventive medication
- Using a copayment plan Let’s say you injure your ankle and visit your primary care physician, who orders an X-ray. It’s just a sprain, so the doctor prescribes a generic pain medication. On the KP 0/25/Rx plan, you would pay a $25 copay for the primary care office visit and a $40 copay for the X-ray.
- Financial Assistance for HIV & PrEP HIV and PrEP medications can be expensive, and for those struggling financially, copay assistance programs may help bridge the gap. Kaiser Permanente coordinates with several manufacturers and foundations to help patients who are eligible and qualify. There is no guarantee of availability.
By Jan Greene
Oakland, Calif. — Researchers have developed a new analytical tool that identifies people at risk of contracting HIV so they may be referred for preventive medication. A study describing the tool was published July 5, 2019, in The Lancet HIV by investigators at Kaiser Permanente San Francisco, the Kaiser Permanente Division of Research, Beth Israel Deaconess Medical Center, and Harvard Medical School.
Looking at medical records of 3.7 million Kaiser Permanente patients, researchers developed a machine-learning algorithm to predict who would become infected with HIV during a 3-year period. The algorithm flagged 2.2% of all patients as high or very high risk; this group included nearly half the men who later became infected, a significant improvement from other published HIV risk prediction tools.
Jonathan Volk, MD, MPH, infectious disease physician, Kaiser Permanente San Francisco Medical Center
“In preexposure prophylaxis, or PrEP, we have an incredibly powerful tool to stop HIV transmission,” said senior author Jonathan Volk, MD, MPH, an infectious disease physician who treats patients with HIV at Kaiser Permanente San Francisco Medical Center. PrEP is a daily antiretroviral pill that is more than 99% effective in preventing HIV.
“It is critical that we identify our patients at risk of HIV acquisition,” Dr. Volk said. “We used our electronic medical record to develop a tool that could be implemented in a busy clinical practice to help providers identify patients who may benefit most from PrEP.”
The Centers for Disease Control and Prevention estimates that just 7% of the people who could benefit from PrEP are taking it. Health care providers have difficulty identifying people at risk for HIV acquisition. Relying on the CDC’s indications for PrEP — sexual orientation and a history of sexually transmitted infections — underestimates risk for some populations, including African Americans, who have relatively high HIV incidence and low PrEP use.
Finding a reliable and automated approach to predict which patients are at risk of HIV infection is a high priority for public health officials. The U.S. Preventive Services Task Force recently gave PrEP therapy its highest, grade A rating and urged researchers to develop tools to identify individuals at risk for HIV.
“Our predictive model directly addresses this gap and may be substantially more effective than current efforts to identify those who may be good PrEP candidates,” Dr. Volk said. He emphasized that it does not replace the clinical judgment of medical providers but could save them time and address misconceptions about HIV risk.
The accuracy of the tool is possible because of Kaiser Permanente Northern California’s comprehensive electronic health records, which track many demographic and clinical data points for its members. “Development of the tool required a setting like KP Northern California that had high-quality individual-level data on enough people to identify new HIV infections, which are rare events,” explained Michael Silverberg, PhD, MPH, from the Kaiser Permanente Division of Research and co-author of the paper.
Michael Silverberg, PhD, MPH, investigator with Kaiser Permanente Northern California Division of Research
The investigators analyzed 81 variables in the electronic health record, finding 44 of them most relevant for predicting HIV risk. A tool that used these 44 variables identified 2.2% of the population as having a high or very high risk of HIV infection within 3 years. This high-risk group included 38.6% of all new HIV infections (46.4% or 32 of 69 men who were diagnosed with HIV during the study period but none of the 14 women).
The tool is limited, as are others, in identifying women at risk of contracting HIV. That’s because risk for females may be dependent on the risk factors of their partners, which are not captured by the variables included in the tool, Dr. Volk explained. The tool also performs less well among patients for whom the electronic health record contains less data (because they are new enrollees or access care less frequently).
The authors compared their new tool with simpler models and found it identified more patients who acquired HIV. Importantly, simpler algorithms were less likely to identify African Americans who became infected, whereas the new tool performed well for both white and African American patients.
While access to a wide variety of patient information is an advantage for Kaiser Permanente, other health care organizations could build similar algorithms using fewer electronic health record variables, Dr. Volk said. The study found simpler models that included only 6 variables still helped identify patients at risk for HIV.
The tool could be incorporated in electronic health record systems to alert primary care providers to speak with patients most likely to benefit from discussions about PrEP. Clinicians could also take this opportunity to explain the availability of drug manufacturer and publicly funded programs that may cover all or part of the drug’s copay cost. The risk thresholds established in this study flagged a small proportion (2.2%) but large number (13,463) of patients over a 3-year period as potential candidates for PrEP based on HIV risk. The study’s authors note that there are no established HIV-risk thresholds for determining PrEP candidacy, and that few of the patients flagged as high risk in this study received PrEP during the study period.
“Embedding our algorithm in the electronic health record could support providers in discussing sexual health and HIV risk with their patients, ultimately increasing the uptake of PrEP and preventing new HIV infections,” said lead author Julia L. Marcus, PhD, MPH, now at Harvard Medical School and Harvard Pilgrim Health Care Institute but formerly of the Kaiser Permanente Division of Research.
The project was supported by the Kaiser Permanente Northern California Community Benefit Research Program, the National Institute of Allergy and Infectious Diseases, and the National Institute of Mental Health.
Co-authors include Stacey Alexeeff, PhD, and Leo B. Hurley, MPH of the Kaiser Permanente Division of Research, and Douglas S. Krakower, MD, of Beth Israel Deaconess Medical Center.
+++
Through providing easy access to medication, fostering community, and offering telehealth opportunities, Kaiser Permanente Northern California is keeping members free from HIV. Pictured above, Truvada, a pill used to reduce the risk of getting HIV.
At Kaiser Permanente Northern California, thousands of members are benefiting from a focused effort to prevent HIV, mainly through preexposure prophylaxis (PrEP), a daily pill that prevents acquisition of the HIV infection.
In a study by Kaiser Permanente Northern California clinicians that was published in the October 2017 issue of Clinical Infectious Diseases, Kaiser Permanente researchers found no new HIV infections among approximately 5,000 patients using PrEP.

“In clinical trials, PrEP reduces the risk of getting HIV from sex by more than 90 percent, and the experience of PrEP use at Kaiser Permanente Northern California suggests that real-world effectiveness may even be much higher than this,” said Jonathan Volk, MD, MPH, physician and epidemiologist at Kaiser Permanente San Francisco. “The fact that we have seen zero new HIV infections among our thousands of patients actively using PrEP highlights how well this medication works when taken.”
Kaiser Permanente Northern California also encourages condom usage in addition to taking PrEP, as condoms help further reduce the risk of HIV and protect against sexually transmitted infections (STIs).
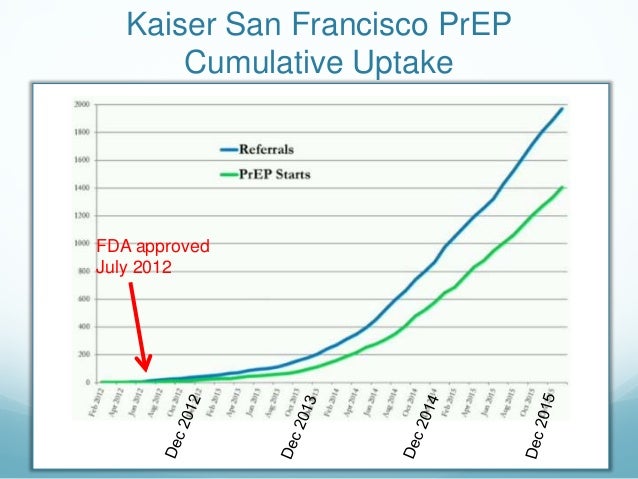
Kaiser Permanente Northern California introduced PrEP, commercially known as Truvada, as a viable option to reduce the risk of contracting HIV almost immediately after the U.S. Food and Drug Administration approved its use in 2012. PrEP is for people who are HIV-negative but at high risk for getting HIV from condomless sex or unsafe injection drug use practices.
How the PrEP Program Works
Members interested in taking PrEP can talk to their Kaiser Permanente primary care physician to get a referral or can self-refer directly to a PrEP-knowledgeable specialist.
Does Kaiser Permanente Cover Prep
Once a member is taking PrEP, the person needs to get quarterly blood tests to check kidney function and for HIV. On the same visit to the lab, patients can self-collect throat and rectal swabs to test for STIs. This self-collection allows patients to get their PrEP follow-up without needing to schedule an in-person appointment. The Kaiser Permanente labs are open on weekends, evenings, and holidays, making it easy and convenient for patients to come in and get the care they need. Patients’ results are then viewable online.
“For the vast majority of our patients, PrEP is tolerated with few or no side effects. It is an incredible tool that we can use to prevent new HIV infections,” said Dr. Volk. “Notably, PrEP is just one of many HIV prevention strategies now available, which also include condoms and making sure our HIV-infected patients are diagnosed and getting treatment.”
Does Kaiser Cover Prep
Levering Technology, Supporting Community
Dr. Volk noted that Kaiser Permanente’s accessible, patient-centered model of health care lends itself to convenient and effective PrEP delivery.
“We provide opportunities for self-collection for STIs, allowing autonomy for our members, and telehealth alternatives to in-person visits. Patients can communicate with their providers at their convenience over secure email or through telephone calls, instead of having to frequently come in for visits that can be challenging to schedule,” said Dr. Volk.
Kaiser Permanente is also leveraging technology to help PrEP patients. Specialized tools on Kaiser Permanente’s computer system allow for effective population management: keeping track of patients who haven’t picked up their medication, are behind on labs, or need additional support or targeted outreach.
‘It Makes Me Feel and Be Safe’
Paul Marcelin has been a Kaiser Permanente member for more than 20 years. A longtime community activist who has led seminars about HIV prevention and currently volunteers on an advisory group for prevention research, Marcelin started taking PrEP in July 2013, once it became widely available. His boyfriend is HIV positive and “undetectable,” meaning that he has no detectable virus in his blood because of his HIV medications; individuals who are HIV-infected and undetectable have a negligible risk of transmitting the infection.
“Kaiser Permanente is night and day ahead of other private providers in terms of HIV prevention,” said Marcelin. “It’s one insurer, one provider, one organization. It’s an integrated system that understands the importance of being open to discussing PrEP, its benefits, and its use.”

Kaiser Prep Copay Card

Marcelin wanted to thank the staff at Kaiser Permanente San Francisco Medical Center, where he receives his care.
“Amazing people work there and they make me feel and be safe. The PrEP program is reducing fear, and people are less afraid to be intimate.”
Tags
Back To TopLook insideKP Northern California is a public-facing news site about Kaiser Permanente Northern California. It is available to physicians and employees, their friends and family, and the public to learn more about the organization and its people.
Read it anywhere, and share it with anyone or on social media!
